Subscribe to Catalyst
Subscribe to get our magazine delivered right to your inbox
Related Articles
They’re called comfort foods for a reason: sugar, salt, and carbs give us a quick boost of flavour and familiarity. Making the case for comforting foods that nourish our mind and body.
“You are what you eat” — We’ve all heard the saying. It’s meant to nudge us toward healthier choices, but it doesn’t reflect all the links between diet and health, including the connections it has with chronic conditions such as diabetes, high blood pressure, obesity, and stroke. It also doesn’t include research over the past 50 years showing how much nutritional choices effect our brain and mental health, which is so striking that we should probably add “Good food for a good mood” to the phrase.

Dr. Bonnie J. Kaplan
Research into the connections between nutrition and mental health began in 1972, when Bonnie Kaplan, then a grad student in experimental psychology, started looking into the physiological and psychological effects of malnutrition during pregnancy and the first few years of life. When she published “Malnutrition and Mental Deficiency” in the Psychological Bulletin that same year, her results struck a chord. She was deluged with requests for reprints of her groundbreaking research, which became the precursor to the field of nutritional psychology. The article’s key takeaway still resonates: “We can’t control our genes, but we can control what we eat so that we can be better nourish our brains and our mental health,” wrote Dr. Kaplan, now a retired research psychologist.
More recently, she co-authored The Better Brain: Overcome Anxiety, Combat Depression, and Reduce ADHD and Stress with Nutrition with Dr. Julia Rucklidge. The book takes a nutrition-first approach to mental health in relation to resilience with a focus on tryptophan — an essential amino acid in the nutrients we can consume — and its connection to serotonin, the “feel-good hormone” that can affect our mood. A short article like this could never fully explain the process of enzymes, co-factors, and chemical reactions involved, but a building-block effect Kaplan describes in her lectures has led her students to the “aha” moment where they can see these connections and are inspired to improve their diet.
The book’s suggestions for healthy eating are by now well known — whole foods (not ultra-processed), fewer carbs, less salt and saturated fats, and a preference for Mediterranean-style cooking — and originate in the “SMILES” trial (2017). In that study, participants with severe depression were randomly placed into two groups, one receiving social support and the other nutrition counselling that recommended a Mediterranean diet of fruits, vegetables, legumes, seafood, olive oil, and seeds. While both groups’ symptoms improved twelve weeks later, people in the Mediterranean diet group saw greater improvement, with 32 per cent of participants’ depressive symptoms going into remission (versus eight per cent for the social support group).
You seem “hangry”
I ask Kaplan: Can you give me a sense of how that happens? Well, she explains, “We cannot eat serotonin in food, right?” Like a rapt student I jot down the key point: “There is no food that contains the feel-good hormone, so we must eat things that enable our bodies to manufacture serotonin and other necessary micronutrients.”
Suddenly, I feel peckish. Chips come to mind — mmmm, all that satisfying salty, carby crunchiness. Except that I also just learned we need at least 30 different micronutrients to properly support our brain’s metabolism, which runs every minute of every day. Such ultra-processed foods can fill our stomach, but they also starve our brain because they’re deficient in vitamins and minerals. It’s the cerebral equivalent of feeling hangry when you’ve waited too long to eat. Kaplan calls this state “hidden brain hunger,” which happens when we consistently lack necessary micronutrients, so the brain lacks what it needs to function optimally and support our mental health. Why is this “hidden”? Because the resulting effects are not always directly felt.
These days, price hikes from inflation make stocking the pantry with such foods a costly challenge for many. Having limited access to fresh foods is also a problem, particularly for those living in food deserts, who must pay even more with the additional time and travel. —
No easy answers
It turns out that our brain is actually the greediest organ in our body: while it accounts for just two per cent of body weight, it absorbs at least 20 percent of all the nutrients we consume, Kaplan says. Feeding that beast means nourishing the brain with micronutrients. Canada’s latest food guide snapshot shows us what this could look like: filling half the plate with a rainbow of fruits and vegetables, and each of the other two quarters with protein and whole grains.
If only it were that simple.
These days, price hikes from inflation make stocking the pantry with such foods a costly challenge for many. According to Food in Canada magazine, grocery prices have spiked more than seven per cent over the past year — the fastest increase in 13 years. Canada’s Food Price Report forecasts that the most significant increases for 2022 will be in the healthy food category, including dairy and vegetables. That means, an average family of four will pay nearly $15,000 for food this year, almost $1,000 more than in 2021. Having limited access to fresh foods is also a problem, particularly for those living in food deserts, who must pay even more with the additional time and travel.
While Kaplan’s findings can tempt us to draw easy parallels between a change in food and mood, depression is a complex state for those who experience it. We should also keep in mind that changes in diet alone are no substitute for seeing our physician or therapist and taking prescribed medications. Still, as the field of nutritional psychology grows, it is helpful to see its recommendations become part of an integrative or alternative treatment for mental health challenges, something that one in five people in Canada live with.
Views and opinions expressed in this article do not necessarily represent the views and opinions of the Mental Health Commission of Canada.
Subscribe to Catalyst
Subscribe to get our magazine delivered right to your inbox
Related Articles
It’s Pride Month! These celebratory events — signature weeks and months, T-shirt days, and other public acknowledgments — provide visibility and a sense of collectivity. Let’s not let the colours fade when the calendar changes.
We skipped toward the main drag with our extended family for some quality time after months apart because of pandemic isolation orders. It was nice to be off screens and among people as we took in the sights on a Sunday in small-town Ontario. This day had all the check marks: great weather, ice cream stands, antique shops, people picnicking, and traffic that halted for jaywalkers zigzagging from shop to shop. At the strip’s entrance was a rainbow crosswalk, providing a highlight for pedestrians entering the busy thoroughfare, and visibility of another kind. Pride crosswalks are designed to promote inclusion and awareness of 2SLGBTQ+ communities, and they range from six-colour rows to chevroned designs that underscore intersecting identities.
Like a lot of municipal infrastructure, this particular project needed an update after a few years of wear and tear. The chipped paint seemed like a bit of handy symbolism as I reflected on Pride Month and many symbolic days and months that bring people together around an issue and idea — which sometimes fade away when the calendar page flips.
The well-being of people with diverse gender identities can be greatly affected by the characteristics, norms, practices, and spaces of our institutional environments. This is reflected in the things we see and the actions we take. —
On this day
“I’m Black all year,” a friend likes to quip as we head into February and she bemoans the litany of requests for very visible speaking engagements, which arrive in the weeks before Black History Month, while offers for secure and steady paid work in her field never materialize. When you experience the gap between a passing visibility and the very real inability to provide for yourself, acknowledgment months can sometimes feel like window dressing. I suppose that’s part of the risk of putting a lot of energy into special months or T-shirt days. But it might also lead us to ask ourselves what contribution is being made. Is it a surface effort? A small step toward systemic change? I’m not ready to write off these events just yet — though their snapshot effect may obscure the complexity of the lived and living experiences in the communities being recognized.
The tagline for GLADD, the American media advocacy organization, says that it “rewrites the script for LGBTQ acceptance.” Its Pride Month Resource Kit for journalists takes a huge step toward this by highlighting some of the pitfalls and assumptions telegraphed through footage and images in Pride events coverage. “No single image should be put forth as representative of either the LGBT community or the range of events that occur at Prides,” it counsels, noting that “colorful and unconventional participants play an important role at Pride events and celebrations.” GLAAD encourages journalists to “avoid the tendency to ignore the diversity that exists at Pride events,” since relying on “outrageous or over-the-top images and footage marginalizes subjects by taking them out of context to depict them as abnormal — perpetuating misconceptions.”
These suggestions bring to mind the drag parade float images of past coverage and lead me to realize how such things can become visual shorthand for progressive movements that are dynamic and complex. Such movements can also quickly become co-opted from their origins in social change. Recent protests to counter “rainbow-washing” — supporting anti-2SLGBTQ+ interests while claiming public allyship with 2SLGBTQ+ communities — have emerged alongside calls to extend Pride initiatives beyond one month, particularly in remote communities.
Representation matters
The well-being of people with diverse gender identities can be greatly affected by the characteristics, norms, practices, and spaces of our institutional environments. This is reflected in the things we see and the actions we take. For the Catalyst, the Mental Health Commission of Canada’s (MHCC’s) online magazine, this means avoiding oversimplification in our storytelling while emphasizing recovery and optimism. We want to offer hope, but not false hope — and no single, tightly construed narratives. In other words, we believe it’s important to recognize the both-and in any given experience — a perspective illustrated in recent COVID-19 research. New Leger polling for the MHCC and the Canadian Centre on Substance Use and Addiction shows that 2SLGBTQ+ communities have faced heightened rates of stigma, discrimination, and harassment during the pandemic yet were also feeling more resilient, hopeful, accepting, and inclusive.
The poll’s other findings reflect a similar complexity. While about one-quarter of 2SLGBTQ+ respondents reported excellent or very good mental health during the pandemic, rates were significantly lower for 2SLGBTQ+ youth, people from low-income households, and those from East and Southeast Asian, South Asian, and African, Caribbean, and Black (ACB) communities. This same pattern was found in connection with the stresses of COVID-19. Though only half of 2SLGBTQ+ respondents reported being able to cope with pandemic stress, fewer 2SLGBTQ+ youth and ACB respondents could do so.
On an individual level, we also have a chance during Pride Month to reflect on its evolution and what it means for Indigenous communities. As well, we might consider why something so seemingly simple as crosswalks are being subjected to defacing and vandalism, thus reducing the visibility of that quiet sign of support. In context of the pandemic, Pride can be a chance to build networks to support 2SLGBTQ+ youth and racialized communities, who are contending more than most with overlapping crises, by being an ally throughout the year.
Subscribe to Catalyst
Subscribe to get our magazine delivered right to your inbox
Share This Catalyst
Related Articles
When older adults make the move into care homes, it becomes essential to forge new bonds. Finding ways through loneliness and isolation with music.
Evidence that strong interpersonal connections are essential to our mental and physical health is growing. And these ties may be more important as we age, particularly among older adults living in retirement residences and long-term care homes. According to Dr. Kristine Theurer, who’s been a researcher in the long-term care sector for more than two decades, “We all yearn to connect with others, and for many people, moving into a residence means seeing friends and family less frequently. So it’s crucial for them to make new connections.”
The harmful effects of social isolation and loneliness on mental and physical health are well known. Several studies have found that isolation increases the risk of cardiovascular disease, obesity, anxiety, and depression and that loneliness can lead to depression, alcoholism, and suicidal thoughts.
During the pandemic, public health measures such as masks, physical distancing, and size limits on gatherings have added to social isolation and loneliness. In retirement and long-term care homes, in‑person visits with family members and volunteers were banned for months, and residents only interacted with staff wearing protective masks, face shields, and gowns.
While these conditions pushed isolation to the limit for these residents, growing public concern was at least able to bring more attention to the issue and give Theurer a chance raise awareness about fostering human connections. A 2015 article she was the lead author on in the Journal of Aging Studies article had already documented the value of standardized peer support and peer mentoring. “The Need for a Social Revolution in Residential Care” argued for an overhaul of programming in retirement residences and long-term care by incorporating activities that advanced residents’ social identities, encouraged reciprocal relationships, and increased social interaction. The goal of that vision was to transform the model of resident care into one of resident engagement — a state that covers basic needs but also allows people to thrive and be enriched.
“Many homes focus on light group activities, such as games and crafts, without recognizing that the crucial benefits actually come from meaningful interactions between peers,” Theurer said. “The focus needs to be on building those meaningful connections.” —
She began harnessing the power of peer support groups and peer mentoring to foster meaningful interactions in 2011, after founding Java Group Programs. The efficacy of the organization’s three research-based programs — Java Music Club, Java Memory Care, and Java Mentorship — has since been demonstrated in a series of studies. Today, hundreds of retirement residences and long-term care homes across North America have implemented them. The most popular is Java Music Club, a peer support activity that focuses on interaction and altruism.
Laura Forsyth, regional manager of life enrichment for Chartwell, a company that runs more than 200 residences across four provinces, has seen its effectiveness firsthand: “For our residents, Java Music is magical,” she said. “I regularly see residents who don’t know one another bond and connect through the program.” After we implemented it in 2014, “Java Music has been so successful that it has influenced Chartwell’s corporate culture. We now emphasize meaningful interpersonal connections in nearly everything we do.”
While preventing social isolation and loneliness might sound easy, it isn’t — especially for older adults struggling to adapt to life in a retirement residence or long-term care home. Most residences and homes don’t offer programming that fosters meaningful connections.
“We still have much to learn about the mental health and well-being of people living in long-term care and how to optimize their quality of life,” said Danielle Sinden, who is the director of the Centre of Excellence in Frailty-Informed Care. Part of Perley Health, which serves a community of more than 600 seniors in long-term care and independent-living apartments, the centre conducts and shares the practical research needed to improve care.
Several of its research projects focus on the mental health and wellness of older adults. One pairs up residents living with Alzheimer’s disease with university students and tracks the results over many visits. Another promotes social connection, emotional health, and meaning in life through an online peer support group. The centre is also evaluating Java Music among a group of residents in long-term care.
“I think there’s something about being a passive recipient of care that fosters loneliness and depression,” said Theurer. “Helping others is a pathway to joy and meaning. Properly designed group programs provide opportunities for people to help their peers. And that makes us feel good.”
Informal caregivers who are concerned about the mental well-being of loved ones can find other strategies to help build connections in the Caring for Older Adults During COVID-19 tip sheet from the Mental Health Commission of Canada and in ongoing research into other aspects of caring for older adults.
Related Articles
This blog post discusses substance use and trauma
What does mental health look like? I think that the answer probably depends. Mental health is not a one-size-fits-all concept. This question was top of mind for me when I recently spoke with community outreach workers of the Breaking the Ice (BTI) program at The 519, a city of Toronto agency dedicated to the health, happiness, and meaningful participation of 2SLGBTQ+ communities.
Breaking the Ice at the 519
Breaking The Ice (BTI) is focused on the needs and barriers faced by 2SLGBTQ+ people who use drugs in Toronto’s Downtown East. Peer-led and rooted in the principles of harm reduction and anti-violence, the team engages in regular street outreach, develops resources targeted to community needs, and supports The 519’s drop-in clients.
Nadine is a BTI coordinator, leading a team working with the people living in the encampments of Toronto. Supporting people who live outside can involve check-ins, providing basic supplies or emotional support, helping with housing or shelter, and it includes the intense work of supporting people who are in conflict with the law. It can also involve responding to people experiencing overdose.
Operating on the block in Toronto that sees one of the most overdoses in the city, harm reduction workers like Nadine are bearing witness every day to suffering and death.
“Nobody should be seeing what we see,” she says. “It’s exhausting. The grief and loss are incredibly heavy – for community, and for folks providing supports.”
Nadine’s experience provides insight into the broader conversations about a post-pandemic return to “normal.” While some sectors of society can talk about getting their lives back, many people are being left behind.
The pandemic significantly impacted the communities served by BTI and created unprecedented challenges for the people supporting them. The crisis shifted everything about their work. The need for housing and shelter was already at a crisis level before the pandemic, but COVID-19 exacerbated the situation. There was a lack of trauma-informed services available and widespread disruptions to health and social service offerings, and minimal access to wrap-around supports. Despite the challenges, The 519 never stopped service provision, and pivoted to an essential service provision model.

Opioid deaths and hospitalizations surged significantly across Ontario after the pandemic hit in early 2020, seriously impacting people who were under or unemployed, precariously housed, or unhoused. In 2021, 2,819 people died from opioid toxicity, an increase from 2,460 opioid deaths the year before, according to data from the Office of the Chief Coroner. These statistics, the BTI team points out, need to be framed with the understanding that many overdoses go unreported.
Nadine and her colleagues worry about the future. They see increasing poverty, evictions, lost employment, worsening affordability, and discrimination affecting more people. Youth are part of the upward trend. In a given year, there are at least 35,000-40,000 youth in Canada who are unhoused or precariously housed, staying with friends, living in “squats,” renting rooms in boarding houses, or are street-involved. Unhoused youth report high rates of alcohol and substance use compared to youth in the general population and are disproportionately exposed to violence with limited access to healthcare.
Indigenous youth and African, Caribbean, and Black youth are over-represented in the numbers of youth affected. Youth who identify as 2SLGBTQ+ make up 25-40% of the youth experiencing homelessness. Trans youth often face unique and complex challenges. As well as discrimination in the shelter system trans youth often face mistreatment and violence. Nadine and the BTI team often witness their communities having to navigate systemic discrimination within shelter environments.
Wellness As Privilege
The statistics and numbers provide context but cannot illustrate what it’s like to try to survive in subsistence mode where access to basics such as water and sanitation is not necessarily a given. As Nadine and her colleagues point out, looking at the situation from a distance with an arms-length perspective, is a position of privilege. “How can we even ask about their wellness and mental health,” says Nadine, “when people are struggling to get their basic needs met? It’s unfair.”
It’s an important question as policy makers grapple with the uneven effects of the pandemic. How can we put physical and mental health on equal footing without addressing systemic barriers and questions of access?
The pandemic has magnified deep social problems that pre-existed it, holding up a mirror to our failings as a society. In April, New York Times op-ed page editor Sarah Wildman underscored this point: “Society has rarely taken the most vulnerable into account when it comes to how daily life is navigated. The irony is, if we made vulnerability less stigmatized, less isolated, less shameful, and invisible… we might be less afraid of it.”
To the people like Nadine who do this work, the fundamental issue of basic human rights is eclipsed by the anti-poverty rhetoric and the invisibility of the substance use crisis in Canada. Yet the pandemic has added another layer of complexity. “The pandemic has been overshadowing this equally important public health crisis, the overdose situation is not being talked about. There is no appetite to hear about it.” The shame and the stigma associated with substance use is divided between socially acceptable and criminal substances. “All social classes use drugs. Find someone who has not been touched by it.” says Nadine.
Showing Up in Meaningful Ways
The 519’s BTI program is based on relationships and consent-based interactions. Supporting people with respect and dignity is based on workers like Nadine being available when and how they are needed and meeting people where they are. “If someone needs five hours of my time, that’s ok”, Nadine says, “but it is challenging in such a high-needs context”.
Doing this work often means reframing our notions of success. For example, when Nadine assisted a client who was experiencing a serious mental health crisis, she assisted the person in getting “formed” – meaning they were voluntarily admitted to a psychiatric facility as an alternative to being incarcerated. (The term “formed” comes from the Form 1 psychiatric assessment that a physician completes to determine if a person needs to be admitted for further care as an involuntary or voluntary patient). In this case, the person was able to access treatment rather than being immediately jailed—meaning they were treated as a person who needed care rather than as a criminal.
Nadine and workers like her see firsthand the effects of stigma and the hyper-criminalization of communities of people who live outside and/or use substances and the attendant cycles of homelessness and incarceration.
Placing human dignity at the centre
According to a growing body of research, a shortage of affordable housing directly contributes to homelessness but so do systems failures that include difficult transitions from child welfare, and inadequate discharge planning for people leaving hospitals, corrections and mental health and substance use treatment facilities.
The common threads of systems failures, stigma, and discrimination seem inextricably intertwined, like a gordian knot. For policy makers attempting to untangle that knot, one thing becomes clear: what is needed is an approach that is rooted in human rights and addresses historic harms, colonialism, and institutional oppression. An approach that is informed by human dignity, rather than perceptions from a perspective of privilege.
When asked how she copes with working on the front lines of the crisis, Nadine says that despite the heavy toll of this work on her own mental health, “knowing what happens is disturbing but not more disturbing than not being there.”
Views and opinions expressed in this blog post belong solely to the original author and do not necessarily represent the views and opinions of the Mental Health Commission of Canada.
Author: Nicole Chevrier
An avid writer and photographer. A first-time author, she recently published her first children’s book to help children who are experiencing bullying. When she isn’t at her desk, Nicole loves to spend her time doing yoga and meditation, ballroom dancing, hiking, and celebrating nature with photography. She is a collector of sunset moments.
Subscribe to Catalyst
Subscribe to get our magazine delivered right to your inbox
Share This Catalyst
Related Articles
There is no strong silent type when it comes to men’s mental health
By Michel Rodrigue
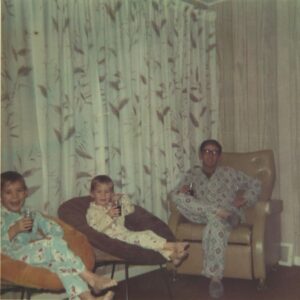
Michel Rodrigue, left, enjoying a soft drink (a treat!) in preparation for the hockey game – the Montreal Canadiens, of course.
Long before I knew what mental health was, I knew that men didn’t talk about it. Certain topics were simply off the table, with deep personal feelings heading the list. To talk about those things would be unnatural, unwelcome, and uncomfortable — not to mention unmasculine.
It was only later, when I learned the concept of stigma, that I understood the truth. When men stay silent, it hurts everyone, most of all themselves.
Of the roughly 4,000 suicide deaths in Canada each year, 75 per cent are men. For men between the ages of 15 and 39, suicide is the second leading cause of death (after accidental death). Clearly, we have a lot to talk about.
Stigma breeds silence
My father worked in construction most of his life. In his all-male crew, if someone was injured on the job, the first aid response was unflinching. There was no hesitation about doing or saying the wrong thing. There was no reassessment of that person’s masculinity or judgment of their character. Everyone understood the reality — that it could have happened to any of them.
In the same way, no one is immune to mental illness. Yet, if someone would have had a panic attack on the job site, I suspect the response would have been entirely different. That’s stigma at work.
But there’s another feature that sets mental illness apart — it’s invisible.
We can see the limp of an injured leg or read the temperature of a fever. Mental health problems, on the other hand, often hide in plain sight. —
I learned this the hard way when I lost a close friend to suicide.
From the outside looking in, Sylvain had everything to live for. A loving wife, two beautiful daughters, a caring family, close friends, and a thriving business. At least, that’s what we thought.
It was only after his death by suicide in May 2005 that we learned he’d been pretending to go to work for many months.
I try to imagine what that time must have been like for him. How ashamed and embarrassed he must have felt to keep that secret so closely guarded. I think about the role stigma played in his death. And I think about how much work we still have ahead of us, especially men.
Turning insights into action
In my seven years with the Mental Health Commission of Canada, I’ve learned a lot about men’s mental health. I’ve learned about the growing evidence of a distinct male-type depression, characterized by externalizing symptoms such as irritability, anger, and substance use.
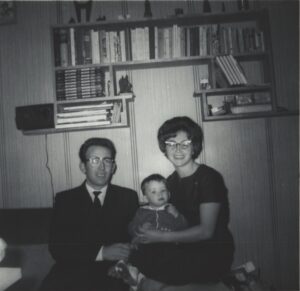
A young Michel with his parents Lionel and Lucille.
I’ve learned that while loneliness, substance use, and depression are among the strongest risk factors for suicidal behaviour in men, other factors put certain subgroups at an even higher risk. For example, the rates of attempted suicide for First Nations, Inuit, and Métis who identify as sexual and/or gender minority men (including gay, bisexual, men who sleep with other men, and transmen) are up to 10 times as high as for men in this group who are non-Indigenous.
But perhaps the most important thing I’ve learned is that, as men, we need to get comfortable being uncomfortable. Talking honestly about our mental health is one of the best ways we can protect it, no matter how unnatural it might feel at first.
At best, the cost of silence is isolation, even in the company of other people who would willingly offer their support. At worst, that silence can cost a life. It’s time for all men to embrace the discomfort, break through the masculine ideals, and leave nothing off the table.
Michel Rodrigue is president and chief executive officer of the Mental Health Commission of Canada.
Michel Rodrigue
Related Articles
I recently took up roller skating.
My legs are sore from my practice session in my cousin’s basement. A seasoned hockey player, he agreed to help me, although he was mostly unconcerned, absentmindedly shooting a tennis ball around as I wobbled.
I’m 26, and I have spent the past few years in a transitive state. I made two major moves during the pandemic and have started from the beginning in foreign places where I know no one.
I need to learn, to feel motivated. I need to have fun in a city where I’ve spent the past eight months in my apartment, going to school, work, therapy and talking to friends despite not leaving the living room.
Mastering roller skating can’t replace my friends or cure growing pains, but that feeling of exhilaration when I begin to glide and feel control makes me excited, makes me smile, even sometimes makes me whoop with triumph.
It won’t fix my existential confusion, but it’s enough for now.
My parents are in an almost opposite stage of life. As I try to find my groove, they struggle to slow down.
I told my mother that there’s a lot to look forward to, and I don’t want her to regret being sad during these years. Each phase of life has something different to offer us, but this transitive stage makes it unbearable to face –– it’s lonely and daunting and the hardest thing I’ve ever had to do.
My parents are clinging to their past selves. They both still work, although they are financially secure, and my father is nearly 70. They’re frustrated that they get tired more, can’t do physical things as easily and need more help. My mother explained that it’s scary, realizing your body is turning on you, and fearing that you will lose the ability to function.
I agreed, shivering at the thought. But I still encouraged her to explore what this phase of life can offer that she and my father haven’t had: total financial security, no responsibility over children, no parents to worry over. They can enjoy what they’ve worked for, they can finally sit back. Their time can be theirs, not their job’s or children’s. They can try new things, rediscover forgotten hobbies, read books in one sitting and stay up until 2AM binging Netflix because they don’t have to work the next day.
It’s hard to accept change. I’m trying to adjust to the crushing responsibility of independence and my parents are trying to prolong their productivity instead of enjoying the results.
While I must lean into my fears, my parents must let themselves relax. We both have joy waiting for us, we just need to reach for it in different ways.
A recent writing and communications student who is slowly settling into her niches of feminism, mental health awareness and editorial writing. She is an avid reader and media consumer, and one of her all-time favourite books is A Tree Grows in Brooklyn. In her spare time, Aishah can either be found drawing or painting in the winter, and camping, canoeing and swimming in the summer.
Subscribe to Catalyst
Subscribe to get our magazine delivered right to your inbox
Related Articles
Showing Support Means Not Having All the Answers
Cuba Gooding Jr. as Rod Tidwell and Tom Cruise as Jerry Maguire from the 1996 film, which led to countless “help me, help you” memes.
A popular quote from the movie Jerry Maguire is, “Help me help you.” It comes from the scene where the namesake character, played by Tom Cruise, is coaching football player Rod Tidwell, played by Cuba Gooding Jr., who is digging in his heels and resisting advice. It’s a familiar exchange that you may recognize in yourself. I know I do. If I see someone in pain, I have the strong desire to jump in and “fix” what I believe to be the “problem.” Despite that desire, I have learned that support does not equal fixing. It’s not my job or your job to fix others.
Let’s start at the point where you have recognized a mental health “problem,” say with a loved one, colleague, or friend. Perhaps you see the signs and symptoms of a decline in their mental well-being, or else the person has told you directly that they are going through a mental health problem. In that moment, it can be tempting to think, “What has worked for me will work for them.” If that happens, it’s natural to want to try and fix things by giving advice on how to make it all better. You may even want to give them a toolbox full of fix-it things.
But there are good reasons not to do that.
“Effective support can also involve sitting beside someone — not speaking a word, simply being there while providing a safe space for them just to be.” —
SHOULDA, COULDA, WOULDA
First, it’s best not to assume we know how that person feels and what they should do. I often say, “Don’t let anyone “should” on you today, and don’t “should” on yourself. So, let’s get away from our preconceived notions of what the person should do.
Whenever I hear the word should, I try to consider where it’s coming from and what intentions are behind it. Who has the right to say what we should do anyway? Who are they to decide what is best?
The desire to fix by “shoulding” ignores other possibilities. What if they’ve already tried what worked for you and had little success? What if it’s the first time someone has really been a witness to their pain? What if they say, “everything is fine,” and go away? What if your timing isn’t their timing (excluding situations of imminent harm to themselves or others)?
A more helpful approach is focusing on how their behaviour is impacting the life they want to live. It’s better to build rapport and trust or encourage them to seek professional (or other) support than put them on your to-do list. They are not your project. And there’s no need to keep at them with questions such as, “Did you do what I told you to do?”
FEELING HUNGOVER
Another potential reaction to trying to fix things is having the person ignore you the next time they see you. Whenever that happens, we tend to blame ourselves: “Did I say something wrong?” “Did I overstep?”
I invite you not to take those thoughts on, since the person may in fact be experiencing shame, denial, or fear. When people disclose something personal and share their emotional pain, it usually leaves them feeling vulnerable.
It’s what I often refer to as the “vulnerability hangover.” They’ve just shared something that leaves them with a gaping emotional hole — that open, raw feeling. In such situations they may be having internal dialogues like, “They must think I’m weird or have a character defect” or “Maybe they don’t like me anymore.”

Yvette Murray
On top of the symptoms they may be experiencing, going through a decline in their mental well-being will affect their self-esteem and self-worth. Strong feelings of “I’m not good enough” or “There must be something ‘wrong’ with me” can rear their ugly heads.
As a psychotherapist, my training involved having to do my own inner work along with group work. One of the biggest “aha” and healing moments I had during that time was when I recognized pain in a colleague or mentor. In that moment I thought, “You mean, you feel this way, too?”
Such an experience provides hope, optimism, and comfort in knowing that someone is not the only one with such feelings. It helps them focus on how to feel better without the extra burden of what my good friend and mentor Janine Driver calls, “stinkin’ thinkin’,” the internal dialogue and self-stigma that can directly interfere with our healing journey.
KNOWING ME, KNOWING YOU
To truly support someone, “Help me help you” really is the best approach. How do we do that? The first step is asking them! For example, ask “How can I best support you?” “What do you think would happen if you did this or that?” “How can I support you today?” “What does help look like for you?”
You could also remind them of what worked for them before. Everyone of us has been through challenges. To overcome them, chances are we’ve used support systems, inner strength, perseverance, courage, and persistence. Reminding the person what they’ve previously come through can be helpful. When someone feels better, they tend to forget that.
Have you ever had a bad flu and thought to yourself, “I don’t know how I’m going to function in the next hour, never mind getting up and going to work the next day”? Fast forward a few weeks, and someone at the office reminds you, “Remember, you were off sick that week?” “Ah, I had forgotten ‘cause now I feel better.” By reminding someone what has helped them before, know that it could be the very thing that helps them now.
Effective support can also involve sitting beside someone — not speaking a word, simply being there while providing a safe space for them just to be. When I don’t feel good, having someone trying to make me feel good or change how I’m feeling can be counter-productive.
Having empathy is key, as American researcher Brené Brown says, while making sure not to jump in with “at least” statements: when someone tells you they are getting a divorce, for example, and you respond with something like, “Well, at least you got married.” Some might find such a comment funny, but it may not be helpful. A more empathetic response would be “Thank you for sharing that with me. Please help me understand what you are going through.”
Key aspects of supporting other people are listening and communicating non-judgmentally. Those things become a lot easier once you remind yourself, “It’s not for me to put my belief systems about how life ‘should’ be or how people ‘should’ act onto others. It’s their life and experience, not mine.” By connecting as an authentic fellow human being, heart to heart, and by really listening, you are going to provide excellent support.
For those that have a hard time receiving support, allow me to whisper in your ear, “know that helping you, helps me too!”
Photo: ©TriStar Pictures/Courtesy Everett Collection
Subscribe to Catalyst
Subscribe to get our magazine delivered right to your inbox
Related Articles
Staying mentally well in a digitized world
While Digital Health Week was a celebration of the advantages of connected care — from virtual consultations to e-health records to useful apps — it was also an opportunity to reflect on how we maintain our best mental wellness in an increasingly digitized world.
“There’s no doubt that the pandemic has increased our reliance on virtual connectivity and social media,” affirmed Dr. Keith Dobson, professor of clinical psychology at the University of Calgary. “And while there are some positives associated with our capacity to remain plugged in to our relationships, we can’t be blind to the very real pitfalls.” —
Those pitfalls are having an especially adverse effect on the mental health and wellness of young people — especially young girls.
“Our brains tend to believe what we can see,” Dobson said. “While intellectually, we might comprehend that a photo is doctored, that an image has been filtered or retouched — a waist nipped in, eyes made bigger — our brain doesn’t readily make that distinction.”
Seeing is believing
Dobson explained that the primacy of our sense of sight is largely why we as a society are so enamoured with digital platforms like Instagram that offer powerful visual stimulants. We’re also reeled in by the hit of dopamine, the feel-good hormone that kicks in when we’re using a medium that offers us easy wins. Likes, hearts, shares, and comments give us bite-sized endorphin rushes, without requiring much in the way of effort.
“Normally, we get a sense of well-being from an accomplishment,” he added. “Something that has required us to invest meaningful time, energy, and effort. Instead, social media provides us with a short-cut. But it’s one that comes at a high cost. The industry we’re up against is a formidable foe — one that has invested billions to buy access to our innermost thoughts and most intimate insecurities.”
Ironically, Dobson noted, we don’t need to feel good while we’re actively engaging on social media. That activity might make us feel less-than, unattractive, not-good-enough. But interestingly, when we shut down our phones, we start to feel good again.
The ‘negative feedback’ loop
“It’s called a negative feedback loop,” he said. “Think of it like this: you have a negative thought — ‘I’ve left the stove on,’ for example. Then you need to check the stove to make sure it’s off. After you find relief in checking, the pattern begins again.”
Holly Craib, a 21-year-old art student in Ottawa, agreed. “I don’t even consciously decide to check my social media. In a moment of boredom, quietness, or loneliness, I just automatically reach for my phone and start scrolling.” She describes the frustration of an hour or two slipping by, checking Twitter or “doom scrolling,” pulling herself up short when she realizes she’s making herself insecure by comparing her accomplishments to those she’s seeing on her feeds.
Dobson echoed Craib’s assessment, explaining that there are myriad things that pull us toward social media. We may fear we’re missing out. Then there’s the pull of social currency: wanting to be sure we can contribute to a conversation about a particular social media event, personality, or meme.
But things can take a dangerous turn when our insecurities are being mined as precious data by organizations seeking to profit from our distress. Eating disorders have increased during the pandemic, and researchers are connecting the link between being in lockdown and having constant access to tempting content that reinforces negative thoughts and damaging behaviours.
A love-hate relationship
“It’s a vicious cycle,” said Craib. “I think like a lot of people my age, I have a love-hate relationship with my phone. I’ll often see friends posting the equivalent of ‘you’ll have to reach me on my landline’ because they are taking a breather from all the noise on social media.”
Once you’ve shown an interest a certain kind of content, algorithms designed to snag your attention quickly respond with reinforcing information. Suddenly, a single search like “How to lose five pounds” becomes a tsunami of diet content. If you weren’t convinced you needed to slim down before that innocuous search, you’re suddenly inundated with the message that you absolutely do.
“And therein lies the danger of being a passive consumer,” said Dobson. “I realize that the tools we have in our arsenal are relatively weak against a billion dollar behemoth that lives in our pocket and seemingly reads our minds, but that’s why we’ve got to be doubly savvy.”
Coming to grips with virtual reality
If you grew up with Seventeen magazine, for example, which you could read and put aside, it may be hard to conceive just how ubiquitous social media’s influence has become. It’s not just the latest trends, funny jokes, and a way to stay in touch with grandma. It’s the whole world in the palm of your hand — and for a lot of young people it becomes their validation, their connection, and their biggest detractor.
Craib said cutting herself off from her phone would be like cutting a lifeline, especially during COVID. “Virtual connection has been part of my life since I was logging on to MSN Messenger when I was in elementary school. I got my Facebook account when I was 13. I don’t know how not to connect with people this way. But I also understand it’s playing on my vulnerabilities, and that’s a fine line to walk.”
Dobson advocates education as the most powerful tool we have — especially for parents of young people. He urges parents to learn about social media and to openly discuss the content their children are seeking, teaching them from an early age how to be critical consumers. “Having them ask, ‘What is the purpose of this image?’ And then, ‘How does it make me feel?’ gives them an opportunity to see if their thoughts are being distorted by unhealthy, unrealistic standards of beauty or accomplishment, for example.”
He also advocates clear boundaries that, he readily admits, won’t necessarily be easy to enforce.
“Some obvious ones for me are no phones in the bedroom, time-limited access to phones and computers, and pursuing other activities that give you an endorphin rush that’s earned without strings attached.”
Learning an instrument, exercising, going for a walk, or having a meaningful conversation with a close friend are social media alternatives that give our brain a feel-good boost, without the inevitable crash.
But for Craib, the work she does as an artist keeps her tethered to the platform she finds most problematic. “Instagram is a natural place to showcase my art, which I love making. But it’s also a forum where you can start to feel unseen, drowned out, or less prolific. I suppose in that way it’s a bit like having a frenemy. On the one hand, you’re able to put yourself out into the world. And, on the other, the world is there to respond.”
Taming the beast
But for April Yorke, there are ways to tame the beast. During her time as the Mental Health Commission of Canada’s manager of digital marketing, she has mastered the skill of making social media work for her, rather than the other way around. And she’s quick to point out that using the platforms can also have positive mental health benefits.
“One of the best things about social media is that it lets you home in on your interests. If you love puppies, fly fishing, and knitting, you can bet you are going to see puppies and fly fishing and knitting, morning till night.”
But if you sense that the algorithm has turned against you (when #HowToLoseFivePounds is all the content you see), Yorke recommends turning the algorithm to your advantage. “Start searching for what makes you happy. When you find it, make sure you like, follow, subscribe, and comment — any action you can take to engage with it. It won’t take long for the algorithm to pick up on where your new interests lie and start pushing you in that direction.”
And if you are still seeing something you don’t like? “Report it. Block the account. Social media gives you those options because they don’t want to show you stuff you don’t want to see and eventually lose you as a customer. Complete the feedback loop by also making it clear what you don’t want.”
Craib is also a proponent of this approach. “I’ve given Twitter a list of words or phrases or subjects a mile long that I am not interested in reading about ad nauseam. It’s not perfect, but it’s a step in the right direction.”
Dialing it back
If those two options aren’t enough, Yorke has another idea. “Act like a feuding celebrity and take yourself back to zero. Unfollow absolutely everyone you are currently following. Remove your own posts and photos that you no longer wish to see.”
Yorke has a friend who took a multi-year break from social media. When he made his return, he used only one network and carefully curated who he was following.
“Now,” said Yorke, “using social media makes him feel inspired in a way that it never did before.”
It’s not usual to see articles recommending strategic avoidance or deleting apps altogether. While that may be the right move for some — it’s not really an option for social media managers or people like Craib, who are required to leverage the connectivity of social media to showcase their work or run a business.
But as Yorke said, “Once you winnow down your list of follows, it doesn’t take as long to ‘get caught up’ (whatever that means), so you spend less time on the app. Now I mostly see my close friends and ads for travel bags with lots of pockets — an important reminder that a big wide world beyond the screen is out there.”
Suzanne Westover
An Ottawa writer and former speechwriter, and Manager of Communications at the Mental Health Commission of Canada. A homebody who always has her nose in a book, she bakes a mean lemon loaf (some would call her a one-dish wonder) and enjoys watching movies with her husband and 14-year-old daughter. Suzanne’s time with the MHCC cemented her interest in mental health, and she remains a life-long learner on the subject.
Illustrator: Holly Craib https://www.hollcee.com/
Subscribe to Catalyst
Subscribe to get our magazine delivered right to your inbox
Related Articles
Putting psychological safety and physical safety on equal footing makes for good policy and practice. A look at changing the narrative within the oil and gas sectors
When the language of isolation, quarantine, and lockdown predominates, there isn’t much room for words like socialize, connect, or empathize. Yet even though the pandemic has made our workplaces more prone than ever to stress and anxiety, creating a culture that gives workers the confidence to ask for mental health support has always been a challenge.
Steve Tizzard knows first-hand what the experience of stigma toward mental health problems at work looks like. He has worked at Hibernia, an oil platform on the Grand Banks of Newfoundland and Labrador, for 25 years and has been front and centre during the company’s shift toward supporting mental wellness.
Tizzard characterizes the earlier stigmatizing attitudes in stark terms:
“You have depression? Go home, you cannot cut it in this industry. You have anxiety? Suck it up, partner, don’t let anyone else hear you say that! Relationship problems? Financial problems? Addiction? All part of the industry. You’re a rough and tumble oil-rig worker; these things cannot affect you!” —As a result, workers often felt they needed to hide their problems and didn’t feel they could ask for help.
Today, of course, these attitudes are giving way. More and more employers understand that mental health problems can affect anyone, no matter what position or industry they’re in, and as Tizzard points out, help is only a conversation away. Teaching workers that it’s OK to let another worker know they’re struggling, having a bad day, or are in crisis — while knowing they will not be judged — is a powerful tool in a workplace.
This simple approach has worked for many Hibernia employees, and its power, Tizzard said, comes from the fact that it is led by workers themselves. Instead of relying on professional supports alone, workers know that others are ready to listen and assist, if necessary. His experience has also taught him that this method may be more effective and immediate than conventional strategies in workplace psychological safety.
He passionately believes in the power of sharing lived experience in open dialogue during workplace safety meetings. “We need to constantly find ways to discuss mental health in the same way as physical health in our workplaces,” he said. By educating workers, saying the words “mental health” in safety meetings and including them in occupational health and safety initiatives, stigma can be reduced.
That said, putting psychological safety on par with physical safety can still be a challenge. As Tizzard puts it, “for some organizations it’s OK to have a sprained ankle but not anxiety. It’s acceptable to bring physical safety issues to the forefront of the workplace agenda but not concerns about psychological safety.”
Despite such challenges, his active support of psychological health and safety at Hibernia has helped it make significant strides. In 2015, the Hibernia wellness committee Tizzard founded was recognized by Canada’s Safest Employers, which awarded the company a gold medal for psychological safety.
When asked what others might look out for when seeking to establish a psychologically safe workplace culture, he said, “any advocate or passionate worker ready to implement a workplace program will need to know it’s not a smooth road much of the time. At first, stigma will always be the main factor in gaining momentum, but the mindset of workers and managers can also hinder success.”
For a program to succeed, Tizzard added, many factors need to line up. What is essential is having a foundation of support from ownership, management, occupational health and safety, and of course, workers themselves. Some of the tools Hibernia is using include micro-learning, wellness boards, and Mental Health First Aid (MHFA) training.
MHFA is a Mental Health Commission of Canada program that teaches people how to offer help to someone who is developing a mental health problem or experiencing a mental health crisis or worsening mental health. Since 2007, almost 600,000 people in Canada have been trained.
According to Tizzard, by combining the right information and skills with an open mind, “trained and caring workers on our shop floors can be so effective in reducing physical and mental injury. It’s an avenue for help that many might not think could exist, but it can be the front-line resource for people in need. I live it every single day.”
Steve Tizzard has worked on the Hibernia platform since 1997, for the last 22 years in a communications, weather, and ice-management capacity. He is the founding member of the offshore wellness committee that serves workers in the oil and gas industry. Apart from the gold medal in psychological safety Hibernia received in 2015, it earned the CM Hincks Workplace Award in 2017 from the Canadian Mental Health Association for excellence in fostering workplace mental health. Steve is also an MHFA instructor and is certified as a psychological health and safety advisor. To learn more about his work, visit www.allthebestconsulting.com.

Nicole Chevrier
An avid writer and photographer. A first-time author, she recently published her first children’s book to help children who are experiencing bullying. When she isn’t at her desk, Nicole loves to spend her time doing yoga and meditation, ballroom dancing, hiking, and celebrating nature with photography. She is a collector of sunset moments.





