Is It Time to Decolonize Therapy?

Subscribe to Catalyst
Subscribe to get our magazine delivered right to your inbox
Related Articles
Subscribe to Catalyst
Subscribe to get our magazine delivered right to your inbox
Related Articles
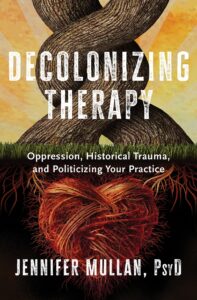
Author Dr. Jennifer Mullan’s new book takes a critical look at care.
There are too many roadblocks to care, resulting in “an outdated system of wellness that is void of wellness.” So says Dr. Jennifer Mullan, a New Jersey-based clinical psychologist and author of the forthcoming book, Decolonizing Therapy: Oppression, Historical Trauma, and Politicizing Your Practice.
According to Mullan, many of those seeking care run into obstacle after obstacle, an experience that reflects what she calls the mental health industrial complex. In response, she has become part of a “growing movement of practitioners who are unlearning colonial methods of psychology,” which seeks nothing less than completely overhauling and restructuring the system.
The book’s 10 chapters are full of scathing observations and critical insight, with titles like “From Lobotomies to Liberations,” “Diagnostic Enslavement,” and “Emotional-Decolonial Work.” Throughout its 400-plus pages, Mullan explores a wide range of problems impairing the mental health system in the United States and elsewhere.
These systems operate like revolving doors, processing many clients but hardly ever dealing with an individual’s pain at the root level. She is convinced that this shortcoming helps explain the spasms of violence erupting with increasing frequency across the U.S., such as school shootings, rising depression levels, and increases in mental health concerns.
Mullan has spent much of her career conducting therapy sessions with children and adults who have experienced domestic violence, unhealthy substance use, child abuse, poverty, and gender identity issues. Over the years, these encounters have chipped away at her optimism and fuelled her frustration.
Ignoring the past
While Mullan’s book examines many different roadblocks to effective treatment, her most blistering criticisms are reserved for the system’s failure to acknowledge intergenerational trauma — which she insists is the root cause of many mental health problems.
She therefore sees her book as “a CALL to ACTION to mental health practitioners, space holders, and wellness workers everywhere. If we are to ‘treat,’ heal, and educate the individual, the group, and/or the organization,” she asks, “is it not essential to also include history, life experiences, and cultural traumas?”
Intergenerational trauma is not a new concept. It gained credence when researchers started studying the impact of the Holocaust perpetrated by Nazi Germany. Nowadays, a growing body of Canadian-led research links the abuse suffered at residential schools with this same kind of trauma. A Historica Canada video describes the experience this way: “For many, the trauma of the mental, physical, and sexual abuse [residential school survivors] suffered hasn’t faded. The children and grandchildren of survivors have inherited those wounds; they have persisted, manifesting as depression, anxiety, family violence, suicidal thoughts, and substance use.” A definition from the American Psychological Association describes how such trauma can make its way across generations. It is “a phenomenon in which the descendants of a person who has experienced a terrifying event show adverse emotional and behavioral reactions to the event that are similar to those of the person himself or herself. These reactions vary by generation.”
Mullan draws heavily on these themes in Decolonizing Therapy, pointing to the history of slavery, internment camps, dictatorships, and residential schools, while arguing that the failure to look at these events dooms future generations to ongoing cycles of pain. Her prescription for therapy means not only exploring family history but probing culture, traditions, rituals, religious beliefs, and practices. Once the buried trauma is revealed, the patient can then receive more focused treatment.
Unfortunately, most therapists are taught almost nothing about revealing intergenerational trauma and are often cautioned against bringing up the past.
“The way many therapists and social workers have been educated,” she says, “is to consistently keep a blank slate, don’t have opinions, don’t have anything in your office that is too forward-facing or political. We’re not going to talk about Black history. We are not going to talk about enslavement. We are not going to talk about racism.”
Waiting and wanting
What is discussed in counselling sessions usually amounts to a short conversation with little time to delve deeper into an issue. Mullan underscores the point by recounting a colleague’s workload at a community clinic that involved more than 90 clients over two weeks. In Mullan’s previous work as a university staff psychologist, she said that nearly 100 students were on a counselling wait-list for six months straight. “Resources have been poorly and criminally allocated,” she says. So, in many settings “money needs to be reallocated.”
A related issue is the crushing workload, which is causing mental and physical health problems for therapists themselves. The book details dismal conditions some therapists are experiencing, such as working other jobs to meet basic needs, paying student loans, dealing with intense vicarious trauma due to the material they are helping to hold, being overworked with up to 80 or more cases a month, moving from job to job, experiencing burnout, and receiving constant microaggressions, bias, and acts of discrimination.
One therapist quoted in the book describes the aftermath of a heart attack she’d had in her office. “It’s not their fault. I thought it was my fault. I changed my diet and worked out more. I went back to work and had panic attacks in between clients. My supervisor told me, ‘You need to get more rest. Are you sleeping? Seeing a therapist of your own?’ No self-care is gonna fix my heart and my anxiety and my nervous system.”
Changing gears
A few years ago, Mullan decided to stop accepting patients and concentrate on reforming the system through public speaking and writing her book, which also lists ideas for deeper reform.
While her views were shaped in the U.S., her calls for change will likely get a thumbs up in many countries. Here in Canada, initiatives like Stepped Care 2.0 are already in place in Newfoundland and Labrador, the Northwest Territories, Nova Scotia, and elsewhere that have radically reduced wait times for mental health services. More organizations are also recognizing Indigenous ways of healing to provide informed and culturally aware forms of therapy. As well, a recent program by the Mental Health Commission of Canada and the Centre for Addiction and Mental Health culturally adapted cognitive behavioural therapy for South Asian communities.
Like many publications covering mental health, Decolonizing Therapy includes exercises, review questions, and detailed references. What makes it stand out is its feisty, passionate, and challenging voice — and Mullan’s personality, which is always present. “I’m holding the Mental Health Industrial Complex accountable and, along with you dear reader, I’m demanding change,” she writes.
Her views are perceived as controversial in certain circles, and some in the profession do not support her activism: a former professor she respects advised her against mixing psychology and politics. Yet Mullan sees it otherwise. In fact, by putting tough topics front and centre, the book is intentionally designed to change that narrative.
Resource: Fact Sheet: Common Mental Health Myths and Misconceptions
Further reading: CBT For You and For Me: A suite of culturally adapted cognitive behavioural therapy tools is designed to break through barriers.




