If you are in distress, you can call or text 988 at any time. If it is an emergency, call 9-1-1 or go to your local emergency department.
- Fact sheets, Research
Rural and remote communities and suicide Fact Sheet
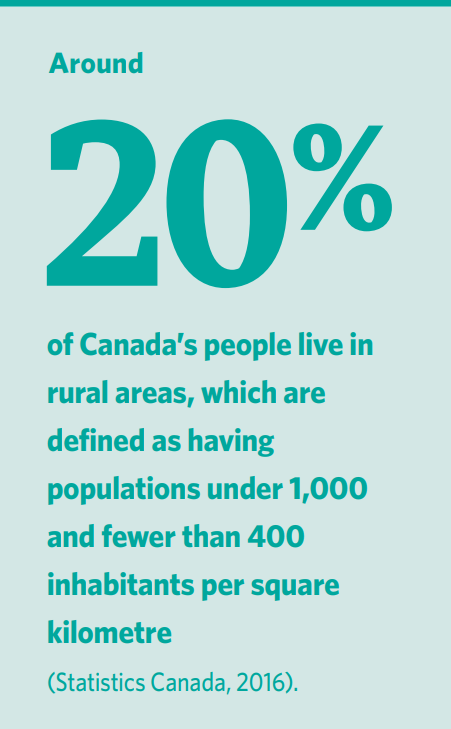
This resource was published in 2022. The data may be out of date. Suicide rates are higher in Canada’s rural areas (Hirsch & Cukrowicz, 2014; Barry et al., 2020). People there also experience poorer health, lower life expectancy, and are less likely to have their healthcare needs met (Eckert et al., 2004) Why are people in rural and remote communities at risk? Certain factors can place some people at a higher risk for suicide than others, and when multiple risk factors outweigh those that build resiliency, the likelihood that a person may think about suicide increases (Sharam et al., 2021). Rural priority populations As outlined below, certain rural and remote populations may be more likely to consider suicide due to additional factors not experienced by others. Governments need to address the mental and physical health needs of these priority populations, and make services for them accessible, i.e., easy to get to, easy to find, confidential, and inexpensive. People who work with these populations should also be trained in suicide prevention.
- Fact sheets, Research
Rural and remote communities and suicide Fact Sheet
Rural and remote communities and suicide Fact Sheet
- Suicide Prevention
This resource was published in 2022. The data may be out of date. Suicide rates are higher in Canada’s rural areas (Hirsch & Cukrowicz, 2014; Barry et al., 2020). People there also experience poorer health, lower life expectancy, and are less likely to have their healthcare needs met (Eckert et al., 2004) Why are people in rural and remote communities at risk? Certain factors can place some people at a higher risk for suicide than others, and when multiple risk factors outweigh those that build resiliency, the likelihood that a person may think about suicide increases (Sharam et al., 2021). Rural priority populations As outlined below, certain rural and remote populations may be more likely to consider suicide due to additional factors not experienced by others. Governments need to address the mental and physical health needs of these priority populations, and make services for them accessible, i.e., easy to get to, easy to find, confidential, and inexpensive. People who work with these populations should also be trained in suicide prevention.
SHARE THIS PAGE
RELATED

Review our Assessment Framework for Mental Health Apps — a national framework containing key standards for safe, quality, and effective mental health apps in Canada.
To help expand the use of e-mental health services, we developed four online learning modules based on our Toolkit for E-Mental Health Implementation, in collaboration with the Centre for Addiction and Mental Health (CAMH).

Stepped Care 2.0© (SC2.0) is a transformative model for organizing and delivering evidence-informed mental health and substance use services.

