If you are in distress, you can call or text 988 at any time. If it is an emergency, call 9-1-1 or go to your local emergency department.
- Reports, Research
Stigma and the Opioid Crisis: Summary
Despite the prevalence of mental illness and substance use across Canada, people who live with such experiences are often still met with stigma. Mental health- and substance use-related stigma can have profound consequences on an individual, especially when it comes from health-care providers and first responders. Such stigma is a major barrier to accessing care, treatment, and recovery and has had a particularly negative impact on those affected by the opioid crisis. Stigma and the Opioid Crisis, a Mental Health Commission of Canada (MHCC) qualitative study, reveals a number of key findings on opioid-related stigma: its character (in the context of direct care and response), impacts, sources, and promising approaches available for tackling it. Social contact reduces stigma by including the personal stories and perspectives of people with lived and living experience of substance use in education, service delivery, policy, research, and training. In the most effective interventions, personal stories and experiences are tailored to reflect and reinforce the program’s main educational objectives. From these findings, the MHCC created the Opening Minds Provider Attitudes Toward Opioid Use Scale (OM-PATOS), which first responder and health- and social-care organizations can use to measure staff attitudes and behaviours and assess the effectiveness of their opioid stigma reduction programs and initiatives. To learn more, visit the MHCC’s Mental Health and Substance Use page.Purpose
Methodology
Key Findings
What opioid-related stigma looks and feels like
Where opioid-related stigma comes from
What impacts opioid-related stigma has
What promising approaches exist for tackling opioid-related stigma
Key recommendations
- Reports, Research
Stigma and the Opioid Crisis: Summary
Stigma and the Opioid Crisis: Summary
- Health-care, Mental Health and Substance Use, Opioids, Stigma
Despite the prevalence of mental illness and substance use across Canada, people who live with such experiences are often still met with stigma. Mental health- and substance use-related stigma can have profound consequences on an individual, especially when it comes from health-care providers and first responders. Such stigma is a major barrier to accessing care, treatment, and recovery and has had a particularly negative impact on those affected by the opioid crisis. Stigma and the Opioid Crisis, a Mental Health Commission of Canada (MHCC) qualitative study, reveals a number of key findings on opioid-related stigma: its character (in the context of direct care and response), impacts, sources, and promising approaches available for tackling it. Social contact reduces stigma by including the personal stories and perspectives of people with lived and living experience of substance use in education, service delivery, policy, research, and training. In the most effective interventions, personal stories and experiences are tailored to reflect and reinforce the program’s main educational objectives. From these findings, the MHCC created the Opening Minds Provider Attitudes Toward Opioid Use Scale (OM-PATOS), which first responder and health- and social-care organizations can use to measure staff attitudes and behaviours and assess the effectiveness of their opioid stigma reduction programs and initiatives. To learn more, visit the MHCC’s Mental Health and Substance Use page.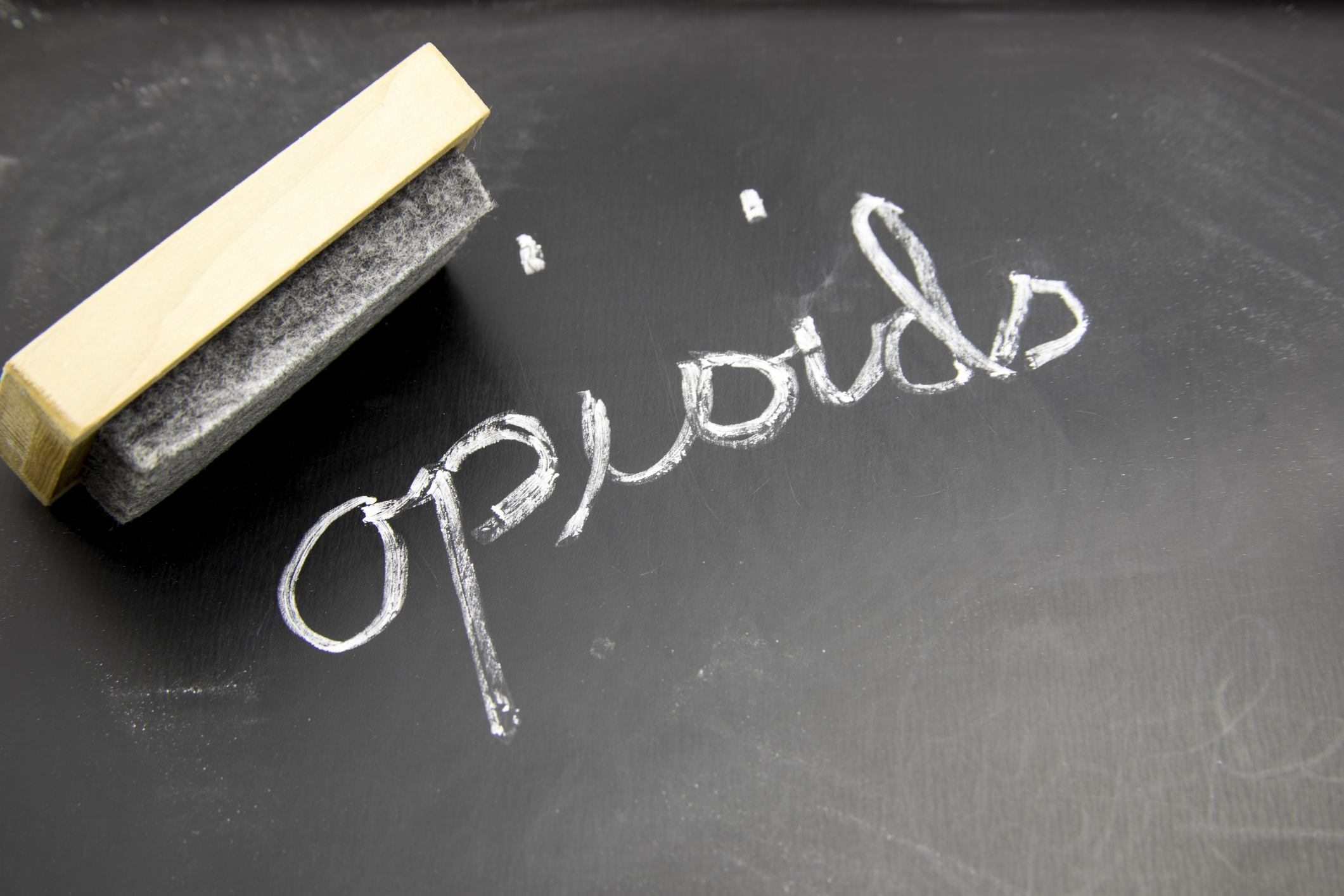
Purpose
Methodology
Key Findings
What opioid-related stigma looks and feels like
Where opioid-related stigma comes from
What impacts opioid-related stigma has
What promising approaches exist for tackling opioid-related stigma
Key recommendations
SHARE THIS PAGE
RELATED

Review our Assessment Framework for Mental Health Apps — a national framework containing key standards for safe, quality, and effective mental health apps in Canada.

To help expand the use of e-mental health services, we developed four online learning modules based on our Toolkit for E-Mental Health Implementation, in collaboration with the Centre for Addiction and Mental Health (CAMH).

Stepped Care 2.0© (SC2.0) is a transformative model for organizing and delivering evidence-informed mental health and substance use services.